Abstract
Background COVID-19 is associated with an increased risk of venous thromboembolism (VTE) and arterial ischemic stroke (AIS) in hospitalized adults. Pediatric data are conflicting with some, but not all studies documenting an increased rate of VTE and AIS in hospitalized children with COVID-19.
Objective The principal objective of the retrospective multicenter study was to estimate the rate of VTE and AIS in hospitalized children between 2018 - 2021, specifically comparing the rate of VTE/AIS during the pre-pandemic years (2018-19) to the pandemic years (2020-21). We additionally investigated clinical presentation and risk factors associated with VTE/AIS during the COVID-19 pandemic.
Methods The study was deemed exempt by the Institutional Review Board at Boston Children's Hospital. Administrative approval was obtained through the Children's Hospital Association (CHA). Data for this study were obtained from Pediatric Health Information System (PHIS), an administrative database that contains clinical and resource utilization data from inpatient, ambulatory surgery, emergency department, and observation encounters for 49-tertiary care children's hospitals in the United States. Data quality and reliability are assured through a joint effort between CHA and participating institutions. International Classification of Disease, 10th Edition, Clinical Modification (ICD-10-CM) codes were used to identify eligible subjects; defined as children (from birth to 21 years of age) hospitalized with VTE and/or AIS between 1/1/2018 - 12/31/2021 at one of 49-participating hospitals. Baseline demographic data, VTE location, and presence of medical comorbidities were also captured using ICD-10-CM codes. T-test (continuous variables) and chi-square test (binary variables) were used to test for association with year (2018-19 vs. 2020-21) or COVID-19 (with vs. without a diagnosis of COVID-19). Analyses were performed using R version 4.0.2.
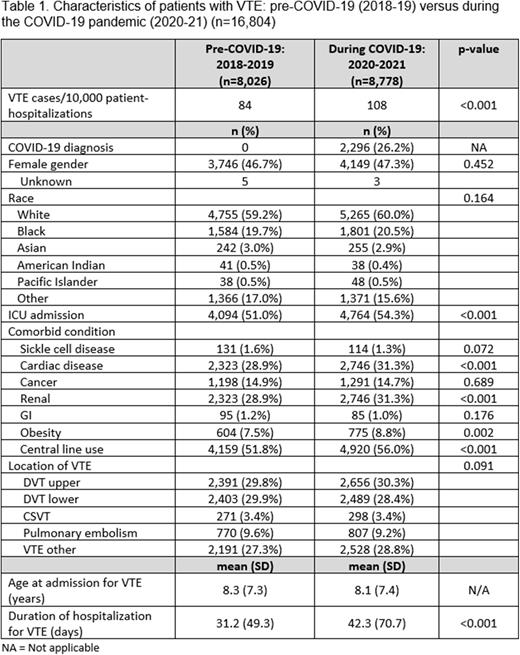
Results During the study period, 1,759,701 unique patients underwent 2,234,135 inpatient hospitalizations. 16,804 (0.95%) patients with a diagnosis code for VTE, and 3,299 (0.19%) patients with a diagnosis code for AIS were included in this analysis. Mean age (standard deviation; SD) at admission was 8.3 (7.2) years, and mean duration (SD) of hospitalization was 35.1 (60.1) days. The VTE rate increased from 84 VTE cases per 10,000 admissions in 2018-19 to 108 VTE cases per 10,000 admissions in 2020-21, representing a 28.6% increase (p<0.001) in VTE events. In contrast, the AIS rate was similar in 2018-19 (19 AIS cases per 10,000 admissions) compared to 2020-21 (18 AIS cases per 10,000 admissions; p=0.1). Clinical characteristics of children diagnosed with VTE prior to/and during the COVID-19 pandemic are summarized in Table 1. Children diagnosed with VTE during the COVID-19 pandemic (2020-21) had longer hospitalizations (p<0.001), were more likely to be admitted to the ICU (p<0.001), and were more likely to have ICD-10-CM codes for congenital cardiac disease (p<0.001) and chronic renal disease (p<0.001), compared to children diagnosed with VTE in 2018-2019.
When only investigating patients admitted during 2020-21, 808,500 unique patients underwent 1,015,951 inpatient hospitalizations. Of the 8,778 (1.09%) patients with VTE, 2,296 (26.2%) patients had a simultaneous diagnosis code for COVID-19. Among children diagnosed with VTE during 2020-21, those who had a simultaneous diagnosis code for COVID-19 were older (p<0.001), more likely to be obese (p<0.001), had longer hospitalizations (p<0.001), and were more likely to have ICD-10-CM codes for congenital cardiac disease (p<0.001) and chronic renal disease (p<0.001) than those without a diagnosis code for COVID-19.
Conclusion Our multicenter observational data shows that the rate of VTE in hospitalized children has risen dramatically during the COVID-19 infection, while the rate of AIS has remained stable. These findings support the need for more effective VTE prevention strategies in children hospitalized with COVID-19.
Disclosures
London:Merck: Consultancy, Other: Data Safety Monitoring Board service; ArQule: Consultancy, Other: Data Safety Monitoring Board service; Jubliant Draximage: Consultancy, Other: Data Safety Monitoring Board service.
Author notes
Asterisk with author names denotes non-ASH members.